New Polymer Fiber Breakthrough Releases Antibacterial Drugs: In recent years, the fight against bacterial infections has taken a significant step forward thanks to innovations in polymer fiber technology that release antibacterial drugs only when needed. This breakthrough represents a promising solution to critical challenges in medicine, such as antibiotic resistance, drug side effects, and inefficient treatment delivery.

Unlike traditional antibacterial treatments that release drugs continuously, these new smart polymer fibers can sense the presence of infection or environmental triggers and deliver medication precisely when and where it is required. This approach not only optimizes therapeutic efficacy but also minimizes risks associated with antibiotic overuse.
This article provides a comprehensive, easy-to-understand guide to this innovative technology, detailing its mechanisms, research findings, real-world applications, and future prospects. Whether you are a healthcare professional, researcher, or simply curious, this article will clarify how this technology works and why it could reshape infection treatment.
New Polymer Fiber Breakthrough Releases Antibacterial Drugs
| Feature | Details |
|---|---|
| Technology Type | Stimulus-responsive smart polymer nanofibers |
| Drug Release Triggers | Temperature, near-infrared (NIR) light, magnetic fields, bacterial presence |
| Core Materials | Polycaprolactone (PCL), graphene oxide, zinc oxide nanoparticles, polyethylene glycol, others |
| Advantages | Targeted antibacterial delivery, reduced side effects, lowered risk of antibiotic resistance |
| Applications | Wound dressings, localized infection treatment, tissue engineering scaffolds |
| Key Research Sources | Royal Society of Chemistry, PubMed, ACS Publications, ArXiv |
| Official Reference Link | RSC Composite Membranes Study |
The new polymer fiber breakthrough that releases antibacterial drugs only when needed represents a major advance in medical materials science. By combining smart, stimulus-responsive polymers with powerful antibacterial agents, this technology offers targeted, efficient, and safer infection treatment.
As research progresses and these materials reach clinical use, they promise to reduce antibiotic resistance, enhance wound healing, and improve patient outcomes significantly. This innovation highlights how smart materials can transform healthcare by delivering therapies more intelligently and precisely than ever before.
What Are Polymer Fibers and Why Are They Important?

Polymer fibers are ultra-thin strands made from long chains of molecules called polymers. Imagine threads thinner than a human hair, which can be spun or woven into mats, membranes, or scaffolds. These materials are widely used in medical devices due to their flexibility, strength, and compatibility with human tissue.
In healthcare, polymer fibers are used for sutures, implant coatings, and wound dressings. Their versatility comes from the ability to modify their structure, chemistry, and physical properties to suit various medical needs.
The Problem with Conventional Antibacterial Treatments
Traditional antibiotic treatments often release drugs indiscriminately throughout the body or continuously at a site. This can lead to:
- Side effects: Such as irritation, allergic reactions, or toxicity.
- Antibiotic resistance: Overexposure encourages bacteria to develop defenses.
- Inefficient treatment: Drugs may reach non-target areas, reducing effectiveness.
Smart polymer fibers aim to overcome these issues by releasing drugs only when and where they are needed.
How Does the New Polymer Fiber Technology Work?
The breakthrough centers on stimulus-responsive polymer fibers that detect specific environmental or biological triggers and release antibacterial drugs accordingly.
Types of Stimuli Triggering Drug Release

- Temperature-Responsive Fibers
Inflammation and infection often cause localized temperature increases. Polymer fibers made from materials like polyurethane or polycaprolactone can change their structure or permeability with temperature shifts, releasing antibacterial agents only when the site warms due to infection. - Near-Infrared (NIR) Light-Triggered Release
Fibers integrated with nanoparticles or phase-change materials can respond to NIR light, which penetrates skin safely and deeply. Doctors can apply NIR light externally to stimulate drug release at precise locations without invasive procedures. - Magnetic Field Activation
Embedding magnetic nanoparticles into polymer fibers allows for drug release controlled by external alternating magnetic fields. This technique offers remote and repeatable activation for on-demand therapy. - Bacteria-Responsive Systems
Some fibers detect bacterial toxins or enzymes and respond by releasing antibacterial drugs. This selective release limits drug exposure to only when pathogens are present, lowering resistance risks.
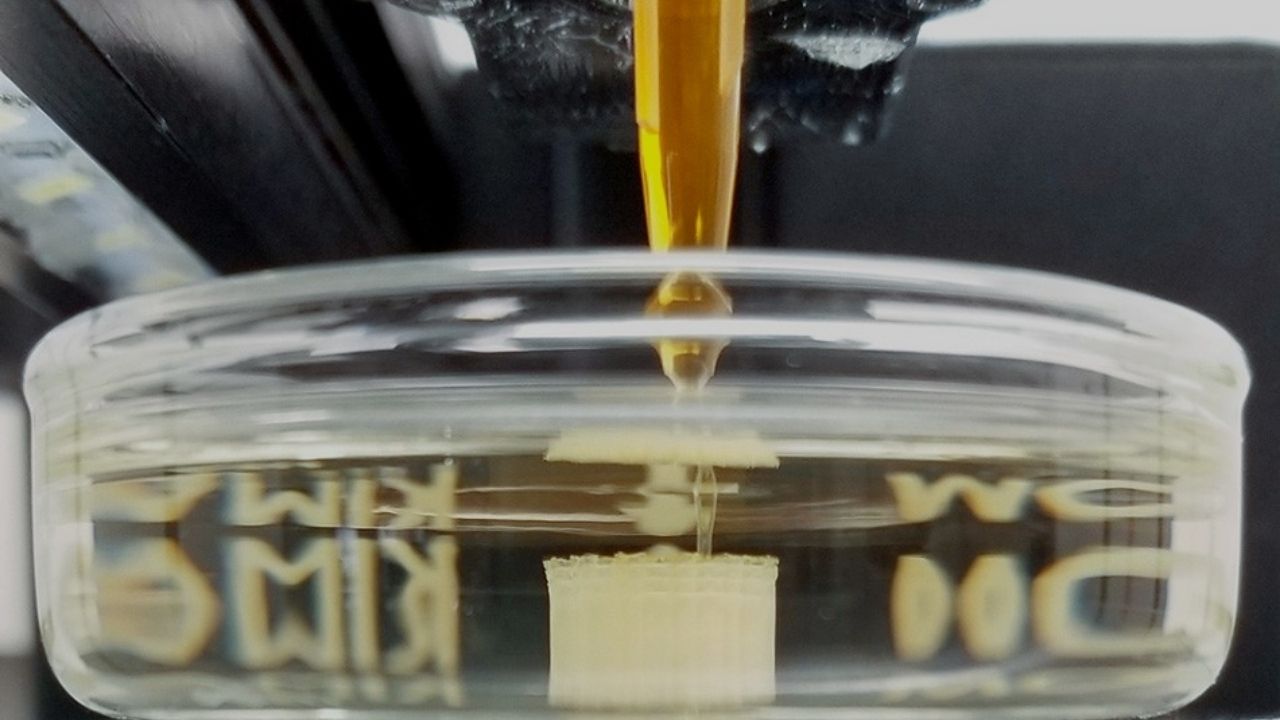
Deep Dive: Polymer Composite Membranes with Shape Memory and Antibacterial Properties
A remarkable example is the composite membrane made of polycaprolactone (PCL) nanofibers combined with graphene oxide (GO), zinc oxide nanoparticles (ZnO NPs), polyethylene glycol (PEG), and the antibacterial alkaloid berberine.
- Shape Memory Effect: The PCL fibers can “remember” and return to their original shape after being deformed. This mechanical property is leveraged to control drug release — stretching or compressing the membrane changes how much drug is released.
- Antibacterial Action: Berberine is an effective natural antibacterial agent. ZnO nanoparticles enhance this effect through their own antimicrobial properties.
- Controlled Release: The composite releases berberine faster under higher mechanical deformation, allowing dosage control through physical manipulation.
This innovative membrane is especially promising for wound dressings, where body movements can regulate drug delivery to infected areas. The research published by the Royal Society of Chemistry in 2024 reports significant antibacterial efficacy against common pathogens such as Staphylococcus aureus and Escherichia coli
Additional Research and Technologies Supporting This Breakthrough
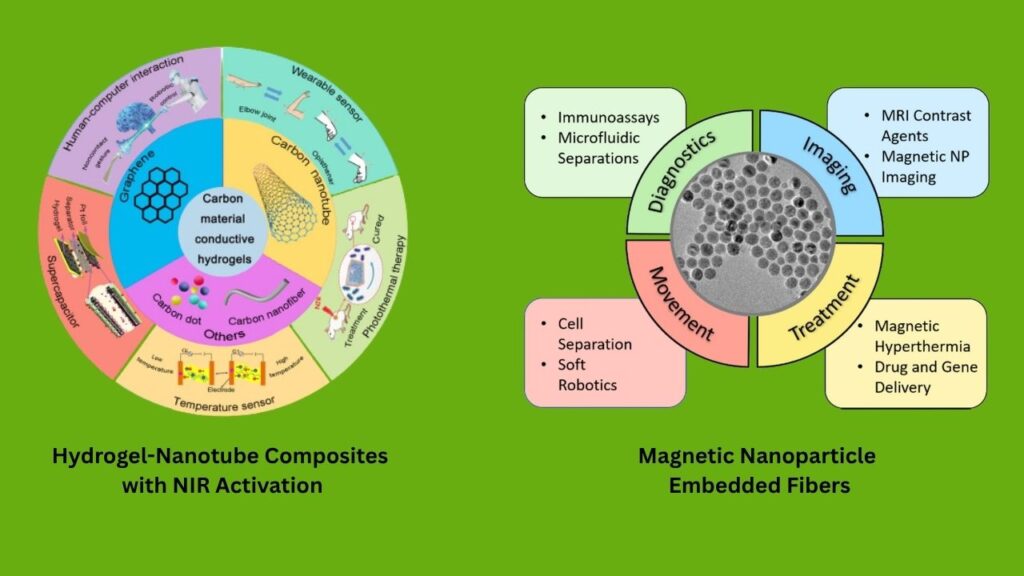
Hydrogel-Nanotube Composites with NIR Activation
Another study demonstrated that hydrogels combined with halloysite nanotubes containing rifampicin (an antibiotic) can release drugs upon NIR laser exposure. The system incorporates a phase-change material that melts and releases rifampicin only when heated by the laser. This technique offers non-invasive, localized infection treatment and is highly promising for skin infections or implant coatings
Magnetic Nanoparticle Embedded Fibers
Electrospun polymer fibers containing magnetic nanoparticles can release drugs like ketorolac or curcumin when subjected to alternating magnetic fields (AMF). This approach enables remote and repeatable on-demand drug delivery without surgery or injections
Practical Applications in Healthcare
Wound Care
Chronic wounds such as diabetic ulcers and burns are particularly susceptible to infection and slow healing. Smart polymer fiber dressings provide:
- Targeted drug delivery activated only by infection markers.
- Reduced dressing changes, improving patient comfort.
- Faster healing by maintaining a moist, antibacterial environment.
Localized Infection Treatment
Implants, catheters, and surgical sites can be coated with these fibers to prevent biofilm formation and infections. By releasing antibiotics only when bacteria begin colonizing, the treatment remains effective while minimizing systemic exposure.
Tissue Engineering
In regenerative medicine, polymer fiber scaffolds that release antibacterial agents help protect newly forming tissues from infection, supporting successful tissue regeneration.
Step-by-Step Guide for Implementing Smart Polymer Fiber Systems in Medical Settings
- Identify Clinical Need
Determine the infection risk and treatment requirements. - Select Appropriate Fiber Technology
Choose polymer fibers based on stimulus responsiveness (temperature, light, magnetic, bacterial). - Prepare and Apply Material
Customize fiber membranes or dressings to patient-specific wounds or implant sites. - Activate Drug Release as Needed
Utilize natural body signals or apply external triggers (e.g., NIR light) to control dosing. - Monitor Healing Progress
Regularly assess wound condition and adjust treatment accordingly. - Allow Safe Degradation or Removal
Most fibers are biodegradable, eliminating the need for removal and reducing patient burden.
Carbon Emissions From Tech Sector Rise With AI Expansion, Report Warns
Precisely Placed Platinum Atoms Boost Catalyst Efficiency and Speed
Ultrasound Technique Accurately Detects Defects in Aluminum Manufacturing
FAQs About New Polymer Fiber Breakthrough Releases Antibacterial Drugs
Q1: How safe are these polymer fibers for human use?
These polymers are made from biocompatible and often biodegradable materials, extensively tested in preclinical studies. However, clinical trials are required before widespread use.
Q2: Can this technology completely replace oral antibiotics?
Not yet. It is a complementary tool designed to optimize and reduce systemic antibiotic use, improving overall treatment strategies.
Q3: What kinds of infections can it treat?
Primarily localized bacterial infections such as skin wounds, surgical sites, and implant-related infections.
Q4: Are there any commercial products currently available?
Several products are in development or clinical trials; broad commercial availability depends on regulatory approvals worldwide.