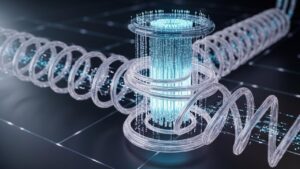
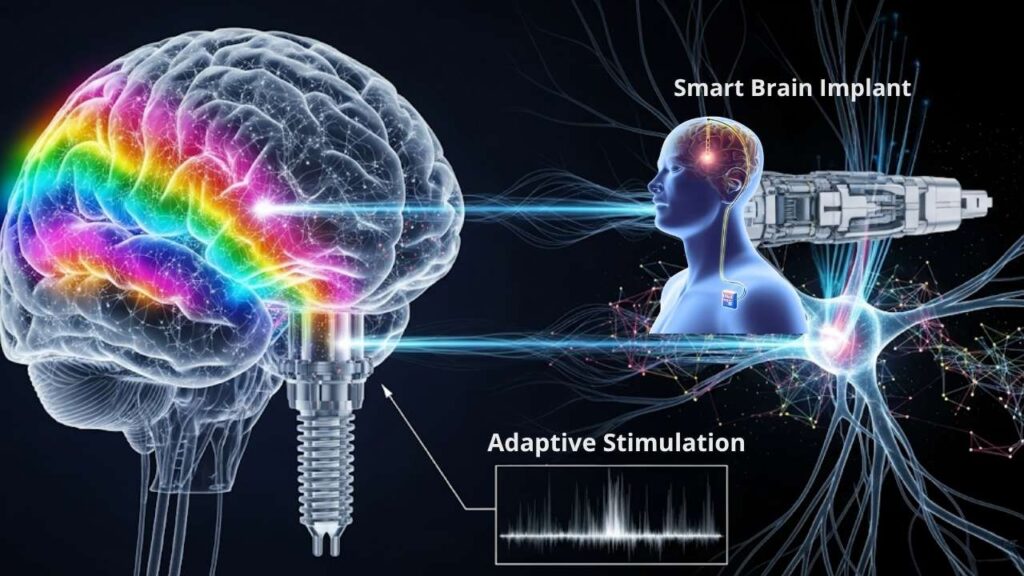
Smart brain implants—devices powered by real-time feedback and artificial intelligence—are revolutionizing how neurologists and patients battle Parkinson’s disease. By understanding a patient’s needs moment by moment and adjusting treatment on the fly, this technology is moving from the realm of science fiction to real-world clinics, offering hope to millions affected by one of the world’s most complex brain disorders.
But what exactly are smart brain implants? How do they work, who are they for, and what can families and professionals expect as these tools go mainstream? In this in-depth article, we break down everything you need to know, from cutting-edge science to practical steps for patients.
Table of Contents
Smart Brain Implants
| Aspect | Details / Insights |
|---|---|
| What Are Smart Brain Implants? | Devices that use AI and sensors to provide brain stimulation only when needed, adapting in real time to changing symptoms. |
| Symptom Improvement | Leading trials show up to 50% reduction in major motor symptoms such as tremor and rigidity, with smoother day/night management. |
| Regulatory Status | First adaptive DBS systems officially approved in early 2025 for clinical use, marking a milestone in personalized therapy. |
| Professional Impact | Requires new, specialized training for neurologists, neurosurgeons, and therapy teams. |
| Practical Advice | Devices adjust automatically, work alongside medications, and can be controlled by the patient for maximum comfort and safety. |
| Broader Potential | Smart implants are being developed to address mood, memory, and even conditions like epilepsy and depression in the future. |
| Official Resource | More information: UCSF Medical Center – Parkinson’s Adaptive DBS |
Smart brain implants—a blend of neuroscience, AI, and sophisticated engineering—represent a new frontier in Parkinson’s disease therapy. Their capacity to tailor therapy in real time, reduce side effects, and potentially address non-motor complications sets a new standard in neurology. As evidence accumulates and expert teams gain experience, more people than ever can look forward to regaining independence, dignity, and hope—one responsive pulse at a time.
The Evolution of Parkinson’s Disease Treatment
Parkinson’s disease is a progressive neurological condition that affects movement, mood, sleep, and thinking. Tremors, stiffness, slowed movement, and lack of coordination are common symptoms. For decades, the backbone of treatment was medication—primarily drugs that replace or mimic dopamine, a crucial brain chemical.
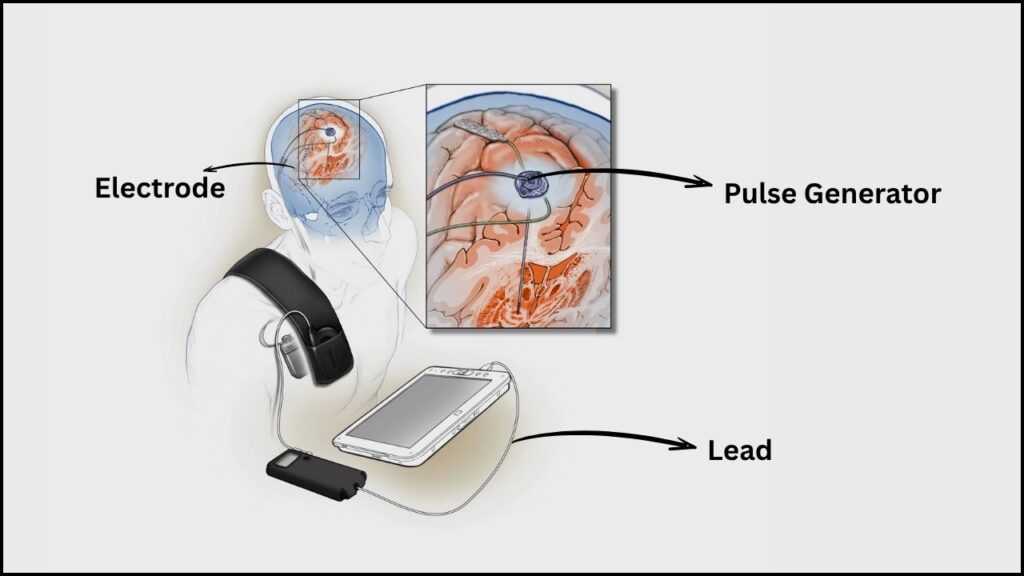
But over time, even the best medication regimens often become less effective. Patients experience unpredictable “on-off” periods—times when symptoms return suddenly or worsen. To better control symptoms, doctors began using deep brain stimulation (DBS). Traditional DBS involves surgically implanting thin electrodes deep in precise brain areas, delivering steady electrical pulses to override abnormal brain activity. While a huge step forward, these conventional devices don’t “think”—they provide the same stimulation all day, regardless of whether symptoms are flaring or not.
What Makes Smart Brain Implants Different?
Adaptive Deep Brain Stimulation (aDBS): A Step Forward
Smart brain implants, also called adaptive Deep Brain Stimulation (aDBS) systems, take DBS technology to a new level. Here’s how they stand out:
- Continuous Sensing: Sensors monitor patterns of brain activity 24 hours a day.
- Real-Time Algorithmic Control: Advanced software—including AI—analyzes these brain signals, spotting early warning signs of returning symptoms.
- Instant Adjustment: Stimulation is increased or decreased automatically, based on need, not on a preset schedule.
- Remote and Patient Control: Devices often feature patient handsets or wireless controls, giving users the ability to pause or override the system when needed for safety or comfort.
Example:
If a patient’s tremor starts to intensify while making coffee, the implant detects this change in brain rhythm and ramps up stimulation within seconds—then eases off when symptoms subside, maybe after a dose of medication.
How Does aDBS Work in Real Life?
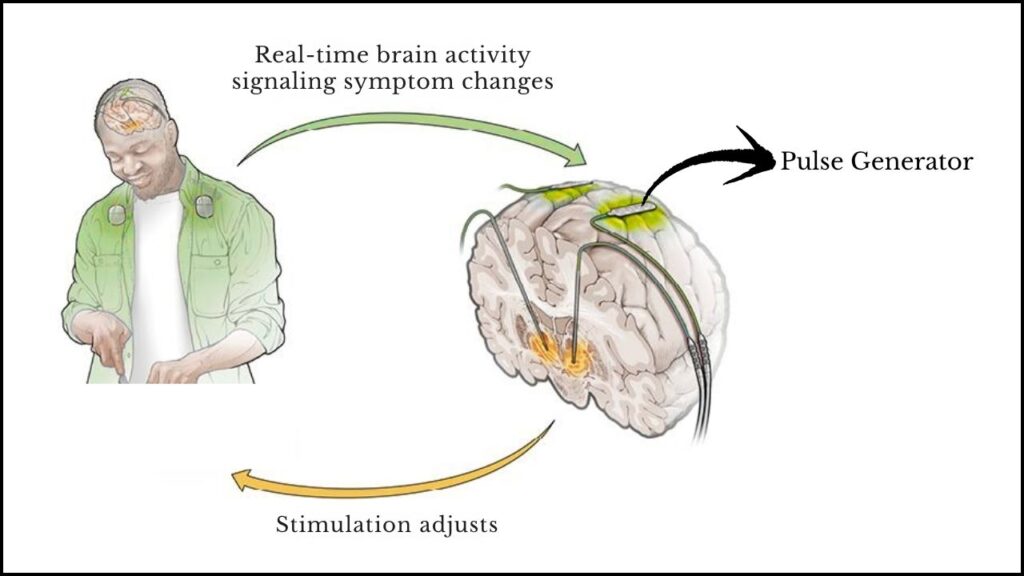
The Decision-Making Loop
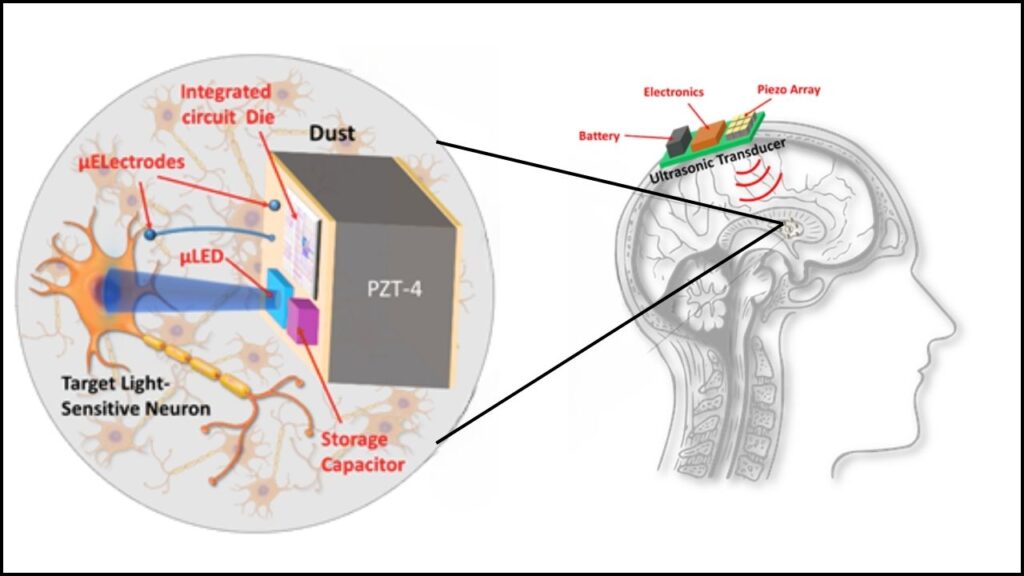
- 1. Detection: The device constantly reads electrical activity from carefully placed sensors in the brain.
- 2. Analysis: AI or pre-trained algorithms flag abnormal patterns linked to symptoms (e.g., increased beta waves signal more movement trouble).
- 3. Action: The system delivers just enough electricity to prevent or relieve emerging symptoms.
- 4. Feedback: It keeps “listening,” always adapting in response to your body, medication cycles, stress, or sleep changes.
What Do Patients Experience?
For many, life with a smart brain implant means steadier movement, shorter and fewer “off” periods—and, importantly, less medication and fewer medication side effects. Many patients find day-to-day tasks, hobbies, and social outings easier. Surprising benefits have been seen for sleep: by recognizing nighttime symptom peaks, the implant makes restless nights less common.
Are the Implants Noticeable?
Most people don’t feel the adjustments—what they notice is reduced shaking, smoother walking, and fewer speech or balance issues. Newer systems are designed for comfort and minimal visibility under the skin.
Clinical Evidence: What Science Tells Us
Landmark Trials & Outcomes
- Symptom Reduction: A pioneering 68-patient, double-blind study showed aDBS can halve the most bothersome Parkinson’s symptom (e.g., tremor or rigidity) compared to traditional DBS.
- Sleep and Non-Motor Benefits: Because the device adapts at night, many reported improved sleep quality, energy, and mood—crucial for overall well-being.
- Lower Side Effects: Adaptive stimulation results in less slurred speech, fewer muscle spasms (dyskinesias), and longer device battery life (since it fires only as needed).
Professional Note:
Medical teams are adapting daily routines to accommodate aDBS. This means longer initial programming sessions, detailed brain mapping, and ongoing algorithm updates. New roles in neurology involve interpreters of neural data, implant programmers, and digital health support staff—a growing career niche.
Real-World Impact: Patient & Family Perspective
A Day in the Life
Meet Rajesh, a 61-year-old retired engineer in India. Years after his diagnosis, medications began losing effectiveness; stiffness and tremors made daily life unpredictable. After being evaluated, he underwent aDBS implant surgery at a leading neurology center. Within weeks, Rajesh could walk with less fear of freezing or falling. He enjoyed a favorite pastime—gardening—and joined his grandchildren without constant worry over symptoms.
His wife notes, “It’s not a miracle cure, but life feels whole again. He’s more positive, sleeps better, and we’re hopeful about the future.”
The Family & Career Angle
Smart implants are not just about symptom management—they help restore independence, allowing many to continue careers or manage family responsibilities longer. This ripple effect touches caregivers, employers, and communities alike.
The Changing Role of Healthcare Professionals
The rollout of smart brain implants demands updated skills and teamwork:
- Training: Doctors must learn to program and fine-tune adaptive systems, which requires understanding complex brain-signal data.
- Teamwork: Success depends on close collaboration between neurologists, neurosurgeons, device specialists, and rehab teams.
- Patient Education: Patients and families learn how to use personal controllers, monitor battery life, and report data for remote adjustments—often with the help of digital health coaches.
- Career Opportunities: As the field grows, roles in digital neuromodulation, algorithm development, and patient care navigation are set to expand.
A Look to the Future: Beyond Parkinson’s
Expanding Potential
- More Than Movement: Clinical and lab trials are investigating whether smart DBS can help mood disorders (like depression), obsessive-compulsive disorder, and epilepsy.
- Next-Gen Implants: Research at UK and US centers involves biohybrid implants—combined living cells and electronics—to repair, not just support, worn-out brain connections.
- Smarter Algorithms: Future devices may use neural network AI to predict a patient’s symptoms hours or days ahead, personalizing care even further.
Step-By-Step Guide: Is Smart Brain Implant Right For You?
Who Might Qualify?
- Diagnosed Parkinson’s, especially moderate-to-advanced stages.
- Symptoms are not well controlled by medication alone.
- Good overall health and able to undergo surgery.
How to Get Started
- Comprehensive Assessment: A neurologist specializing in movement disorders will assess your symptoms, brain imaging, and medication history.
- Surgical Planning: Using advanced brain-mapping and imaging, your surgical team plans where to place sensors.
- Procedure: Electrodes are placed in the brain; a small battery is implanted in the chest.
- Programming & Tuning: Over several clinic visits, the system is tailored and calibrated to your unique rhythms and needs.
- Home Management: Some systems keep doctors updated by sending encrypted data directly from your home.
- Ongoing Updates: Algorithms can be upgraded over time as more is learned about your symptom patterns.
Safety & Insurance
Most major medical centers follow strict safety protocols; risks are similar to other minor brain procedures (infection, bleeding, rare device failure). Insurance coverage is improving, especially since regulatory agencies have officially approved the first aDBS devices for standard use.
Side-by-Side Comparison: Conventional vs. Smart Adaptive DBS
| Aspect | Conventional DBS | Smart Adaptive DBS (aDBS) |
|---|---|---|
| Stimulation Pattern | Constant | Responsive, real-time |
| Personalization | Clinic-based adjustments only | Continuous, automatic, AI-driven |
| Device Longevity | 3–5 years (typical) | Often longer due to lower battery use |
| Symptom Control | Good but variable | More even, with less fluctuation |
| Applicable Conditions | Movement disorders | Movement + mood, cognition, epilepsy (future potential) |
| Patient Interaction | Limited | Patient can pause/switch off for comfort/safety |
| Side Effects | More frequent over time | Lower, thanks to precision targeting |
Neuroscientists Decode Visual Signals in Brains of People Without Mental Imagery
Israeli Scientists Reveal the World’s First Brain-Like AI Chip That Teaches Itself
Scientists Uncover Rare Brain Activity That Could Unlock New Frontiers in Human Consciousness
FAQs About Smart Brain Implants
1. Is a smart brain implant a cure for Parkinson’s?
No—a cure remains elusive. aDBS is a treatment that provides better symptom control, giving patients more good days and a higher quality of life.
2. How soon can patients see benefits?
Most patients notice symptom improvement within days to weeks of device activation and tuning. Fine-tuning can continue over several months.
3. Are there risks with the surgery?
Risks are similar to traditional DBS: infection, bleeding, and rare device problems. Doctors take extensive precautions to keep risks low.
4. Will the device be visible? Can it be felt?
The battery pack may be slightly visible/feelable under the skin of the chest, but the brain leads are hidden and not felt after recovery.
5. What happens if symptoms change in the future?
The aDBS system can be remotely updated or reprogrammed as your symptoms evolve or as better algorithms become available.
6. Will insurance cover it?
Coverage is growing rapidly since regulatory bodies approved these systems for standard care, but always confirm with your provider.
7. What about people with milder symptoms?
Typically, surgery is reserved for those whose symptoms aren’t well-managed by medication. Early-stage patients usually continue with non-surgical care.